Congratulations on your pregnancy journey! Proper nutrition during pregnancy is one of the most important gifts you can give your growing baby and yourself. This comprehensive guide provides evidence-based information to help you make informed nutritional choices throughout your pregnancy, ensuring optimal health for both you and your little one. From essential nutrients to meal planning strategies, we'll cover everything you need to know for a healthy, well-nourished pregnancy.
Table of Contents
- 1. Pregnancy Nutrition Fundamentals
- 2. Essential Nutrients for Pregnancy
- 3. Prenatal Vitamins & Supplements
- 4. Healthy Weight Gain Guidelines
- 5. Nutrition by Trimester
- 6. Pregnancy Meal Planning
- 7. Foods to Avoid During Pregnancy
- 8. Managing Common Pregnancy Symptoms
- 9. Special Dietary Considerations
- 10. Preparing for Postpartum Nutrition
1. Pregnancy Nutrition Fundamentals
Pregnancy nutrition goes far beyond "eating for two." It's about providing your body and your developing baby with the right nutrients at the right times to support healthy growth and development. Your nutritional needs change throughout pregnancy, and understanding these changes is key to maintaining optimal health.
Why Pregnancy Nutrition Matters
Proper nutrition during pregnancy supports:
- Fetal development: Brain, organ, and tissue formation
- Maternal health: Energy levels, immune function, and recovery
- Birth outcomes: Healthy birth weight and reduced complications
- Long-term health: Reduced risk of chronic diseases for both mother and child
- Breastfeeding preparation: Building nutrient stores for lactation
Key Principles of Pregnancy Nutrition
Quality Over Quantity
While you do need additional calories during pregnancy, the focus should be on nutrient-dense foods that provide maximum nutritional value. Choose whole, minimally processed foods whenever possible.
Gradual Caloric Increase
Contrary to popular belief, you don't need extra calories in the first trimester. Caloric needs increase gradually:
- First trimester: No additional calories needed
- Second trimester: Additional 340 calories per day
- Third trimester: Additional 450 calories per day
💡 Smart Calorie Additions
Use our Calorie Calculator to determine your baseline needs, then add the appropriate amount for your trimester. Focus on nutrient-dense additions like Greek yogurt with berries, avocado toast, or a handful of nuts.
Consistent Nutrient Intake
Your baby's development happens continuously, making consistent daily nutrition more important than occasional "perfect" meals. Aim for balanced nutrition throughout each day and week.
Understanding Nutritional Changes
Pregnancy brings significant physiological changes that affect nutrition:
- Increased blood volume: Requires more iron and fluid
- Hormonal changes: Affect appetite, digestion, and nutrient absorption
- Growing uterus: May compress stomach, affecting meal size
- Metabolic changes: Alter how your body processes nutrients
- Placental development: Creates additional nutritional demands
🌟 Your Pregnancy Nutrition Goals
Focus on providing optimal nutrition for fetal development while maintaining your own health and energy. This means emphasizing nutrient-dense foods, staying hydrated, taking prenatal vitamins, and listening to your body's changing needs throughout pregnancy.

2. Essential Nutrients for Pregnancy
Certain nutrients become especially important during pregnancy due to their critical roles in fetal development and maternal health. Understanding these key nutrients and their food sources helps ensure you're meeting both your needs and your baby's.
Folic Acid (Folate)
Why it's crucial: Prevents neural tube defects and supports DNA synthesis
Daily need: 600-800 mcg
Best sources: Fortified cereals, leafy greens, legumes, citrus fruits, asparagus
Timing: Most critical in early pregnancy, ideally starting before conception
Iron
Why it's crucial: Supports increased blood volume and prevents anemia
Daily need: 27 mg (nearly double pre-pregnancy needs)
Best sources: Lean red meat, poultry, fish, beans, fortified cereals, spinach
Absorption tip: Pair with vitamin C-rich foods and avoid with calcium or tea
Calcium
Why it's crucial: Builds baby's bones and teeth, maintains maternal bone health
Daily need: 1,000 mg (1,300 mg for teens)
Best sources: Dairy products, fortified plant milks, leafy greens, sardines, tofu
Important note: If intake is inadequate, baby will draw calcium from maternal bones
Protein
Why it's crucial: Supports rapid fetal growth and maternal tissue expansion
Daily need: Additional 25g above pre-pregnancy needs (about 71g total)
Best sources: Lean meats, poultry, fish, eggs, dairy, legumes, nuts, seeds
Distribution: Aim for protein at each meal and snack
Additional Critical Nutrients
| Nutrient | Daily Need | Key Functions | Best Food Sources |
|---|---|---|---|
| Omega-3 DHA | 200-300 mg | Brain and eye development | Fatty fish, walnuts, flaxseeds, algae supplements |
| Vitamin D | 600 IU | Bone development, immune function | Fortified milk, fatty fish, sunlight exposure |
| Choline | 450 mg | Brain development, neural function | Eggs, meat, fish, dairy, cruciferous vegetables |
| Iodine | 220 mcg | Thyroid function, brain development | Iodized salt, dairy, seafood, seaweed |
| Zinc | 11 mg | Immune function, protein synthesis | Meat, shellfish, legumes, seeds, nuts |
| Vitamin B12 | 2.6 mcg | Nervous system, red blood cell formation | Animal products, fortified foods |
Nutrient Absorption and Interactions
Enhancing Nutrient Absorption
- Iron + Vitamin C: Citrus fruits, tomatoes, or bell peppers with iron-rich foods
- Calcium + Vitamin D: Fortified dairy products or supplements taken together
- Fat-soluble vitamins: Take vitamins A, D, E, K with healthy fats
Avoiding Nutrient Inhibitors
- Iron absorption blockers: Coffee, tea, calcium supplements, whole grains (separate timing)
- Calcium absorption blockers: Excessive fiber, oxalates in spinach
- Folate destroyers: Excessive heat, light, and air exposure
⚠️ Nutrient Deficiency Warning Signs
- Iron deficiency: Fatigue, pale skin, cold hands/feet, unusual cravings
- Folate deficiency: Fatigue, irritability, poor concentration
- Calcium deficiency: Muscle cramps, numbness, tingling
- Protein deficiency: Excessive swelling, slow wound healing
Consult your healthcare provider if you experience these symptoms.
Meeting Nutrient Needs Through Food
Sample Daily Nutrient-Dense Menu
- Breakfast: Fortified cereal with milk and berries (folate, calcium, vitamin C)
- Snack: Greek yogurt with nuts (protein, calcium, healthy fats)
- Lunch: Spinach salad with grilled chicken and chickpeas (iron, protein, folate)
- Snack: Apple with almond butter (fiber, healthy fats, protein)
- Dinner: Salmon with sweet potato and broccoli (omega-3s, vitamin A, folate)
- Evening: Glass of fortified plant milk (calcium, vitamin D)
🥗 Nutrient Density Strategy
Choose foods that provide multiple nutrients per serving. For example, eggs provide protein, choline, vitamin D, and B vitamins all in one food. Use our Macro Calculator to ensure you're meeting your protein needs while getting essential nutrients.
3. Prenatal Vitamins & Supplements
While a balanced diet should be your primary source of nutrients, prenatal vitamins serve as important insurance to fill potential gaps in your nutrition. Understanding what to look for in prenatal vitamins and when additional supplements might be needed ensures optimal nutrition throughout pregnancy.
Why Prenatal Vitamins Are Important
Even with the best dietary intentions, meeting all nutritional needs through food alone can be challenging during pregnancy. Prenatal vitamins help ensure adequate intake of critical nutrients, especially during early pregnancy when morning sickness might limit food intake.
Key Benefits:
- Provide consistent daily nutrition regardless of appetite changes
- Ensure adequate intake of nutrients difficult to get from food alone
- Support healthy fetal development from conception through birth
- Help prevent nutritional deficiencies that could affect pregnancy outcomes
- Provide peace of mind about nutritional adequacy
Essential Components of Prenatal Vitamins
🔍 What to Look for in Prenatal Vitamins
| Nutrient | Recommended Amount | Why It Matters |
|---|---|---|
| Folic Acid | 400-800 mcg | Prevents neural tube defects |
| Iron | 18-27 mg | Prevents anemia, supports blood volume |
| Calcium | 200-300 mg | Bone and tooth development |
| Vitamin D | 400-600 IU | Calcium absorption, immune function |
| DHA | 200-300 mg | Brain and eye development |
| Choline | 200-450 mg | Brain development (often missing from prenatals) |
When to Start Prenatal Vitamins
Ideally, start taking prenatal vitamins at least one month before trying to conceive. This ensures adequate nutrient stores, particularly folate, which is crucial for early fetal development that occurs before many women know they're pregnant.
Timeline Recommendations:
- Pre-conception: Start 1-3 months before trying to conceive
- First trimester: Continue throughout, especially important for folate
- Second and third trimesters: Maintain consistent intake
- Postpartum: Continue while breastfeeding
Types of Prenatal Vitamins
Standard Prenatal Vitamins
Most over-the-counter prenatal vitamins contain the basic essential nutrients. Look for third-party tested brands and check that they meet your specific needs.
Prescription Prenatal Vitamins
Your healthcare provider might prescribe specific prenatal vitamins if you have:
- Severe morning sickness affecting nutrient absorption
- Specific nutritional deficiencies
- Dietary restrictions (vegetarian, vegan, food allergies)
- Multiple pregnancies (twins, triplets)
- History of neural tube defects
Specialized Formulations
- Gummy vitamins: Easier to tolerate but may lack iron and have added sugars
- Liquid vitamins: Good for those with swallowing difficulties
- Whole food vitamins: Made from concentrated foods, may be gentler on stomach
- Vegan prenatal vitamins: Plant-based sources, important for vegetarian mothers
💊 Taking Prenatal Vitamins Effectively
- Take with food to reduce nausea and improve absorption
- If iron causes constipation, try taking with vitamin C or switching formulations
- Take at the same time daily to establish a routine
- If you miss a dose, take it when you remember, but don't double up
- Store in a cool, dry place away from children
Additional Supplements to Consider
Omega-3 Fatty Acids (DHA/EPA)
Why needed: Many prenatal vitamins don't contain adequate DHA
Recommended dose: 200-300 mg DHA daily
Best sources: Fish oil or algae-based supplements for vegetarians
Vitamin D
Why needed: Many women are deficient, especially in northern climates
Recommended dose: 1000-2000 IU daily (in addition to prenatal)
Best form: Vitamin D3 (cholecalciferol)
Probiotics
Why beneficial: Support digestive health and may reduce risk of complications
Recommended strains: Lactobacillus and Bifidobacterium species
Timing: Can be taken throughout pregnancy
Choline
Why needed: Often missing from prenatal vitamins despite importance
Recommended dose: 450 mg daily
Food sources: Eggs, meat, fish (supplement if intake is low)
⚠️ Supplements to Avoid During Pregnancy
- High-dose vitamin A: Can cause birth defects (avoid >3000 mcg)
- Herbal supplements: Many are not safe during pregnancy
- High-dose vitamin E: May increase bleeding risk
- Weight loss supplements: Not appropriate during pregnancy
- Energy drinks/supplements: Often contain unsafe ingredients
Always consult your healthcare provider before taking any supplements beyond prenatal vitamins.
Managing Prenatal Vitamin Side Effects
Common Side Effects and Solutions:
- Nausea: Take with food, try different brands, or take at bedtime
- Constipation: Increase fiber and water intake, consider iron-free options temporarily
- Large pill size: Try gummy, liquid, or smaller tablet formulations
- Metallic taste: Take with citrus juice or try different brands
- Stomach upset: Take with meals or try whole food-based vitamins
Quality and Safety Considerations
Choosing Quality Prenatal Vitamins:
- Look for third-party testing (USP, NSF, or ConsumerLab)
- Check expiration dates and proper storage requirements
- Verify the company has good manufacturing practices
- Read labels carefully for allergens and additives
- Choose reputable brands with transparent ingredient sourcing
🩺 Working with Your Healthcare Provider
Discuss your prenatal vitamin choice with your healthcare provider, especially if you have specific dietary restrictions, health conditions, or are taking medications. They may recommend specific brands or additional supplements based on your individual needs and blood test results.

4. Healthy Weight Gain Guidelines
Appropriate weight gain during pregnancy is crucial for both maternal and fetal health. The amount of weight you should gain depends on your pre-pregnancy BMI, overall health, and whether you're carrying multiples. Understanding healthy weight gain patterns helps ensure optimal outcomes for you and your baby.
Why Healthy Weight Gain Matters
Appropriate weight gain during pregnancy supports:
- Fetal growth: Provides energy and nutrients for healthy development
- Maternal health: Supports increased blood volume and breast tissue changes
- Birth outcomes: Reduces risk of complications during delivery
- Postpartum recovery: Easier return to pre-pregnancy weight
- Long-term health: Reduces risk of obesity and diabetes for both mother and child
Weight Gain Recommendations by Pre-Pregnancy BMI
📊 Institute of Medicine Weight Gain Guidelines
| Pre-Pregnancy BMI Category | BMI Range | Total Weight Gain | Weekly Gain (2nd & 3rd Trimester) |
|---|---|---|---|
| Underweight | Less than 18.5 | 28-40 lbs | 1-1.3 lbs/week |
| Normal Weight | 18.5-24.9 | 25-35 lbs | 0.8-1 lb/week |
| Overweight | 25-29.9 | 15-25 lbs | 0.5-0.7 lbs/week |
| Obese | 30 or higher | 11-20 lbs | 0.4-0.6 lbs/week |
📏 Calculate Your Pre-Pregnancy BMI
Use our BMI Calculator to determine your pre-pregnancy BMI category and appropriate weight gain range. Remember, these are guidelines - your healthcare provider may recommend different targets based on your individual circumstances.
Weight Gain Pattern Throughout Pregnancy
First Trimester (Weeks 1-12)
- Expected gain: 1-4 pounds total
- What's happening: Minimal fetal growth, possible morning sickness
- Focus: Maintaining nutrition despite nausea, taking prenatal vitamins
- Note: Some women lose weight due to morning sickness - this is usually not concerning
Second Trimester (Weeks 13-27)
- Expected gain: Steady weekly gain based on BMI category
- What's happening: Rapid fetal growth, increased appetite
- Focus: Consistent, nutrient-dense eating, regular physical activity
- Note: This is often when women feel best and appetite returns
Third Trimester (Weeks 28-40)
- Expected gain: Continued steady gain, may slow near term
- What's happening: Continued fetal growth, maternal tissue expansion
- Focus: Maintaining nutrition despite physical discomfort
- Note: Weight gain may plateau in the last few weeks
Where the Weight Goes
🤰 Breakdown of 30-Pound Weight Gain
- Baby: 7-8 pounds
- Placenta: 1-2 pounds
- Amniotic fluid: 2 pounds
- Uterus: 2 pounds
- Breast tissue: 2 pounds
- Blood volume: 4 pounds
- Fluids in maternal tissue: 4 pounds
- Maternal fat stores: 7 pounds
This shows that most pregnancy weight gain serves important physiological functions.
Factors Affecting Weight Gain
Individual Factors:
- Pre-pregnancy weight and BMI
- Age: Younger mothers may need more weight gain
- Height: Shorter women may gain less, taller women more
- Activity level: More active women may need additional calories
- Multiple pregnancies: Twins require 37-54 pounds gain
- Medical conditions: Diabetes, hypertension may affect recommendations
Pregnancy-Related Factors:
- Morning sickness severity
- Food aversions and cravings
- Gestational diabetes
- Preeclampsia or other complications
- Medications that affect appetite
Managing Healthy Weight Gain
Strategies for Appropriate Weight Gain:
🍎 Healthy Weight Gain Tips
- Focus on nutrient density: Choose foods that provide maximum nutrition per calorie
- Eat regular meals: Don't skip meals, which can lead to overeating later
- Stay active: Regular, moderate exercise supports healthy weight gain
- Monitor portions: Use smaller plates and pay attention to hunger cues
- Stay hydrated: Sometimes thirst is mistaken for hunger
- Get adequate sleep: Poor sleep can affect hunger hormones
If You're Gaining Too Quickly:
- Review your food choices - focus on whole foods over processed
- Check portion sizes and eating frequency
- Increase physical activity if approved by your healthcare provider
- Keep a food diary to identify patterns
- Discuss concerns with your healthcare provider
If You're Not Gaining Enough:
- Add healthy, calorie-dense foods (nuts, avocados, olive oil)
- Eat more frequent, smaller meals
- Include protein and healthy fats at each meal
- Consider nutritional supplements if recommended
- Address any underlying issues (nausea, food aversions)
⚠️ When to Be Concerned About Weight Gain
Contact your healthcare provider if you experience:
- Sudden weight gain (more than 2 pounds in a week)
- No weight gain for several weeks in second/third trimester
- Excessive weight gain despite healthy eating
- Weight loss in second or third trimester
- Swelling in face, hands, or feet with rapid weight gain
Special Considerations
Multiple Pregnancies (Twins, Triplets)
- Twins: 37-54 pounds for normal BMI
- Higher caloric needs: Additional 600 calories/day by second trimester
- Earlier weight gain: More gain in first and second trimesters
- Closer monitoring: More frequent check-ups and assessments
Adolescent Pregnancy
- May need weight gain at upper end of range
- Still growing themselves, requiring additional nutrients
- Higher risk of inadequate weight gain
- Need for specialized nutritional counseling
Gestational Diabetes
- May require modified weight gain goals
- Focus on blood sugar control through diet
- Regular monitoring of weight and glucose levels
- Coordination between healthcare providers
🎯 Remember: Quality Over Quantity
While monitoring weight gain is important, focus primarily on eating nutritious foods and maintaining healthy habits. Your body is designed to support pregnancy, and with proper nutrition and prenatal care, most women gain an appropriate amount of weight naturally.

5. Nutrition by Trimester
Each trimester of pregnancy brings unique nutritional needs and challenges. Understanding what to expect and how to adapt your nutrition throughout pregnancy helps ensure optimal health for both you and your developing baby.
🌱 First Trimester (Weeks 1-12): Foundation Building
The first trimester is crucial for organ development and establishing healthy pregnancy habits, even though your baby is still very small. This period often brings challenges like morning sickness and food aversions.
Key Nutritional Priorities:
- Folic acid: Critical for neural tube development (400-800 mcg daily)
- Prenatal vitamins: Ensure consistent nutrient intake despite nausea
- Hydration: Combat dehydration from morning sickness
- Small, frequent meals: Manage nausea and maintain blood sugar
- Protein: Support early tissue development
Common Challenges and Solutions:
🤢 Managing Morning Sickness
- Eat before getting up: Keep crackers by your bed
- Small, frequent meals: Every 2-3 hours to prevent empty stomach
- Ginger: Tea, candies, or supplements may help nausea
- Cold foods: Often better tolerated than hot foods
- Bland carbohydrates: Toast, rice, bananas, applesauce
- Avoid triggers: Strong smells, spicy or fatty foods
Food Aversions and Cravings:
- Work around aversions: Find alternative sources of key nutrients
- Honor safe cravings: Your body may be signaling nutrient needs
- Don't force foods: Aversions often resolve in second trimester
- Focus on what you can eat: Any nutrition is better than none
First Trimester Meal Ideas:
- Breakfast: Fortified cereal with milk, toast with almond butter
- Snack: Greek yogurt with honey, banana with peanut butter
- Lunch: Chicken noodle soup, crackers, fruit smoothie
- Snack: Cheese and crackers, herbal tea
- Dinner: Baked potato with cheese, steamed vegetables
⚠️ First Trimester Red Flags
Contact your healthcare provider if you experience:
- Inability to keep food or fluids down for 24 hours
- Weight loss of more than 2 pounds
- Signs of dehydration (dizziness, dark urine, dry mouth)
- Severe abdominal pain or cramping
🌸 Second Trimester (Weeks 13-27): The Golden Period
Often called the "golden trimester," this period typically brings renewed energy and appetite. Your baby is growing rapidly, and your nutritional needs increase significantly.
Key Nutritional Changes:
- Increased calories: Add 340 calories per day
- Higher protein needs: Support rapid fetal growth
- Iron focus: Blood volume expansion requires more iron
- Calcium emphasis: Baby's bones and teeth are developing
- Omega-3 fatty acids: Critical for brain and eye development
Nutritional Priorities:
- Balanced meals: Include protein, complex carbs, healthy fats, and vegetables
- Iron-rich foods: Lean meats, beans, fortified cereals, spinach
- Calcium sources: Dairy, fortified plant milks, leafy greens
- Healthy snacks: Support increased energy needs
- Hydration: Increased blood volume requires more fluids
Sample Second Trimester Daily Menu:
| Meal | Food Choices | Key Nutrients |
|---|---|---|
| Breakfast | Oatmeal with berries, nuts, and milk | Fiber, antioxidants, protein, calcium |
| Mid-Morning | Greek yogurt with granola | Protein, probiotics, complex carbs |
| Lunch | Quinoa salad with chickpeas and vegetables | Complete protein, fiber, folate, iron |
| Afternoon | Apple slices with almond butter | Fiber, healthy fats, protein |
| Dinner | Grilled salmon, sweet potato, broccoli | Omega-3s, vitamin A, folate, fiber |
| Evening | Whole grain cereal with milk | B vitamins, calcium, protein |
💪 Second Trimester Energy Boosters
- Regular meals: Don't skip meals to maintain steady energy
- Complex carbohydrates: Provide sustained energy release
- Iron-rich foods: Prevent fatigue from anemia
- Stay active: Moderate exercise boosts energy levels
- Adequate sleep: Support your body's increased demands
🌺 Third Trimester (Weeks 28-40): Final Preparations
The third trimester brings rapid fetal growth and preparation for birth and breastfeeding. Physical discomfort may affect eating, requiring strategic meal planning.
Key Nutritional Adjustments:
- Additional calories: Increase to 450 extra calories per day
- Smaller, frequent meals: Accommodate reduced stomach capacity
- Continued iron focus: Prevent anemia before delivery
- Adequate protein: Support final growth spurt
- Preparation for breastfeeding: Build nutrient stores
Common Third Trimester Challenges:
🤰 Managing Physical Discomfort
- Heartburn: Smaller meals, avoid spicy/acidic foods, eat slowly
- Constipation: Increase fiber and water, gentle exercise
- Reduced appetite: Focus on nutrient-dense foods
- Swelling: Limit sodium, elevate feet, stay hydrated
- Difficulty sleeping: Avoid large meals before bed
Strategic Eating for Comfort:
- 6-8 small meals: Instead of 3 large meals
- Liquid nutrition: Smoothies, soups, milk-based drinks
- Easy-to-digest foods: Avoid foods that cause discomfort
- Upright eating: Sit up straight during and after meals
- Timing matters: Larger meals earlier in the day
Third Trimester Nutrient-Dense Snacks:
- Protein smoothie: Greek yogurt, fruit, spinach, protein powder
- Trail mix: Nuts, seeds, dried fruit
- Hummus and vegetables: Easy to digest, nutrient-dense
- Cheese and whole grain crackers: Protein and complex carbs
- Avocado toast: Healthy fats and fiber
Preparing for Labor and Delivery:
- Stay well-hydrated: Support increased blood volume
- Maintain iron stores: Prepare for potential blood loss
- Build energy reserves: Complex carbohydrates and healthy fats
- Support immune function: Vitamin C, zinc, adequate protein
- Prepare for breastfeeding: Continue prenatal vitamins
🎯 Trimester-Specific Supplement Considerations
- First trimester: Focus on folic acid and prenatal vitamins
- Second trimester: Add DHA if not in prenatal, monitor iron levels
- Third trimester: Continue all supplements, consider probiotics
- Throughout: Vitamin D if deficient, choline if not in prenatal
Always consult your healthcare provider before adding or changing supplements.
📊 Track Your Nutrition Journey
Use our Calorie Calculator to adjust your daily needs for each trimester, and our Macro Calculator to ensure adequate protein intake throughout pregnancy. Regular monitoring helps ensure you're meeting your changing nutritional needs.

6. Pregnancy Meal Planning
Effective meal planning during pregnancy ensures consistent nutrition, saves time and energy, and helps manage pregnancy symptoms. A well-structured approach to meal planning can make healthy eating easier throughout your pregnancy journey.
Benefits of Pregnancy Meal Planning
- Nutritional consistency: Ensures daily intake of essential nutrients
- Symptom management: Helps plan around nausea, heartburn, and food aversions
- Energy conservation: Reduces daily decision-making when energy is low
- Budget-friendly: Reduces food waste and impulse purchases
- Family preparation: Establishes healthy eating patterns for growing family
- Stress reduction: Eliminates "what's for dinner?" anxiety
Pregnancy Meal Planning Principles
The Pregnancy Plate Method
🍽️ Building Your Pregnancy Plate
- 1/2 plate: Colorful vegetables and fruits
- 1/4 plate: Lean protein sources
- 1/4 plate: Whole grain carbohydrates
- Plus: Healthy fats (avocado, nuts, olive oil)
- Plus: Calcium-rich foods (dairy or fortified alternatives)
- Plus: Adequate hydration throughout the day
Meal Timing Strategies
- First trimester: Small, frequent meals to manage nausea
- Second trimester: Regular meal schedule with healthy snacks
- Third trimester: Smaller, more frequent meals due to reduced stomach capacity
- Throughout: Don't skip meals to maintain stable blood sugar
Weekly Meal Planning Process
Step 1: Assess Your Week
- Review your schedule for busy days and appointments
- Consider your current pregnancy symptoms
- Note any food aversions or cravings
- Plan for prenatal appointments and potential fatigue
- Consider partner's schedule and family needs
Step 2: Plan Your Meals
- Start with dinner: Often the most complex meal
- Add breakfast and lunch: Focus on nutrient density
- Include snacks: Plan 2-3 healthy snacks daily
- Consider leftovers: Plan meals that provide multiple servings
- Add variety: Include different proteins, grains, and vegetables
Step 3: Create Your Shopping List
- Organize by store sections (produce, dairy, meat, pantry)
- Include quantities needed for each recipe
- Add prenatal vitamins and any needed supplements
- Include pregnancy-safe snacks and comfort foods
- Don't forget hydration options (water, herbal teas)
Step 4: Meal Prep Strategies
- Batch cooking: Prepare large quantities of staples
- Component prep: Wash, chop, and portion ingredients
- Freezer meals: Prepare meals for busy days or postpartum
- Snack prep: Portion nuts, cut vegetables, prepare yogurt parfaits
- Emergency meals: Keep simple, nutritious options on hand
Trimester-Specific Meal Planning
🤢 First Trimester Meal Planning
Focus: Managing nausea and food aversions while ensuring adequate nutrition
Planning Strategies:
- Plan simple, bland meals that are easy to prepare
- Include foods you can tolerate even when nauseous
- Prepare snacks in advance for quick access
- Have backup options for days when nothing sounds appealing
- Focus on foods rich in folic acid and B vitamins
Sample First Trimester Weekly Plan:
| Day | Breakfast | Lunch | Dinner | Snacks |
|---|---|---|---|---|
| Monday | Toast with almond butter | Chicken noodle soup | Baked potato with cheese | Crackers, ginger tea |
| Tuesday | Fortified cereal with milk | Turkey sandwich | Rice with steamed vegetables | Banana, yogurt |
| Wednesday | Smoothie with protein powder | Vegetable soup with crackers | Grilled chicken with rice | Apple sauce, cheese |

🌟 Second Trimester Meal Planning
Focus: Maximizing nutrition during the period of best appetite and energy
Planning Strategies:
- Include a variety of nutrient-dense foods
- Plan more complex meals while energy is higher
- Batch cook and freeze meals for third trimester
- Experiment with new healthy recipes
- Focus on iron-rich and calcium-rich meal combinations
Second Trimester Meal Ideas:
- Breakfast: Vegetable omelet with whole grain toast
- Lunch: Quinoa bowl with roasted vegetables and chickpeas
- Dinner: Salmon with sweet potato and asparagus
- Snacks: Trail mix, Greek yogurt parfait, hummus with vegetables
🤰 Third Trimester Meal Planning
Focus: Smaller, frequent meals that are easy to digest and nutrient-dense
Planning Strategies:
- Plan 6-8 smaller meals instead of 3 large ones
- Include easy-to-digest, nutrient-dense options
- Prepare freezer meals for postpartum period
- Focus on foods that don't trigger heartburn
- Plan liquid nutrition options (smoothies, soups)
Third Trimester Meal Structure:
- Early morning: Light snack (crackers, fruit)
- Breakfast: Protein-rich, moderate portion
- Mid-morning: Nutrient-dense snack
- Lunch: Balanced, smaller portion
- Afternoon: Protein and healthy fat snack
- Early dinner: Light, easy-to-digest meal
- Evening: Small snack if needed
Pregnancy-Friendly Meal Prep Ideas
Make-Ahead Breakfast Options:
- Overnight oats: Prepare 5 jars for the week with different toppings
- Egg muffins: Bake with vegetables and cheese, freeze individually
- Smoothie packs: Pre-portion frozen fruits and vegetables
- Chia pudding: Prepare in advance, add fresh fruit before eating
- Whole grain muffins: Bake with added protein and vegetables
Batch-Cooked Components:
- Proteins: Grilled chicken, hard-boiled eggs, cooked beans
- Grains: Brown rice, quinoa, farro
- Vegetables: Roasted vegetables, steamed broccoli, sautéed spinach
- Sauces: Pesto, tahini dressing, tomato sauce
Freezer-Friendly Meals:
- Soups and stews: Lentil soup, vegetable stew, chicken soup
- Casseroles: Lasagna, enchiladas, baked ziti
- Individual portions: Burrito bowls, pasta dishes
- Postpartum meals: One-pot meals, slow cooker recipes
🛒 Smart Pregnancy Shopping Tips
- Shop when you feel best: Usually mid-morning for many pregnant women
- Bring snacks: Prevent low blood sugar while shopping
- Use grocery pickup: Save energy, especially in third trimester
- Stock pregnancy-safe staples: Pasteurized cheeses, cooked deli meats
- Buy pre-cut vegetables: Save prep time when energy is low
Managing Meal Planning Challenges
When Nothing Sounds Good:
- Keep a list of "safe" foods that you can usually tolerate
- Have simple backup meals ready (soup, toast, crackers)
- Focus on getting some nutrition rather than perfect nutrition
- Try different temperatures and textures
- Don't force foods that make you feel worse
When You're Too Tired to Cook:
- Use your freezer meal stash
- Rely on simple assembly meals (sandwich, salad, yogurt parfait)
- Use healthy convenience foods (rotisserie chicken, pre-cut vegetables)
- Ask for help from partner, family, or friends
- Consider healthy meal delivery services
🍽️ Remember: Flexibility is Key
Pregnancy meal planning should reduce stress, not create it. Be flexible with your plans, listen to your body's changing needs, and remember that some nutrition is always better than no nutrition. Focus on progress, not perfection.
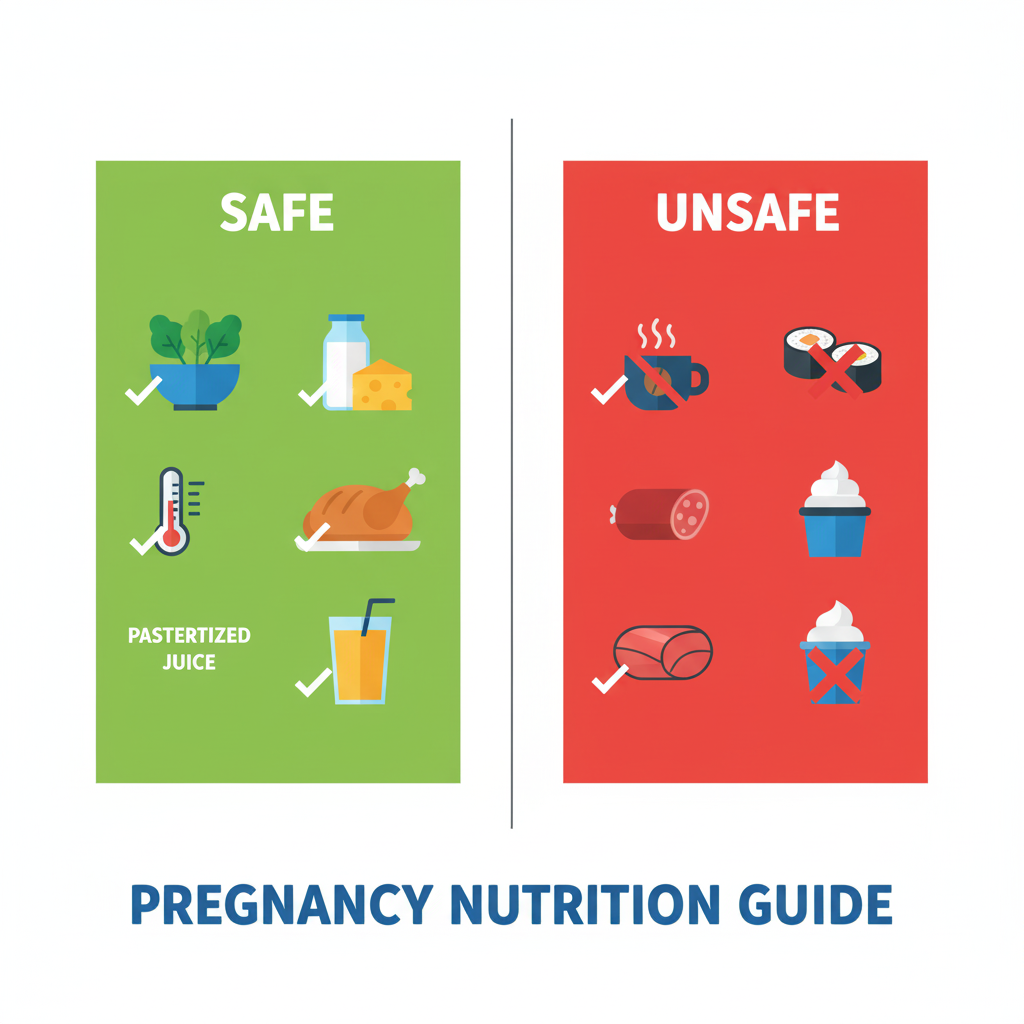
7. Foods to Avoid During Pregnancy
While most foods are safe during pregnancy, certain foods pose potential risks to you and your developing baby. Understanding which foods to avoid and why helps you make informed choices while still enjoying a varied and satisfying diet.
Why Some Foods Are Restricted
During pregnancy, your immune system is naturally suppressed to prevent your body from rejecting the baby. This makes you more susceptible to foodborne illnesses that could harm both you and your baby. Additionally, some substances can cross the placenta and affect fetal development.
Main Concerns:
- Foodborne pathogens: Bacteria, viruses, and parasites
- Toxic substances: Mercury, alcohol, excessive caffeine
- Harmful chemicals: Pesticides, additives, contaminants
- Allergens: Substances that could cause severe reactions
High-Risk Foods to Avoid Completely
🚫 Never Safe During Pregnancy
Raw or Undercooked Animal Products:
- Raw fish: Sushi, sashimi, ceviche, raw oysters
- Raw or undercooked meat: Rare steaks, raw ground meat
- Raw eggs: Cookie dough, homemade mayonnaise, eggnog
- Unpasteurized dairy: Raw milk, soft cheeses (brie, camembert, feta)
High-Mercury Fish:
- Shark, swordfish, king mackerel, tilefish
- Large tuna (limit albacore to 6 oz/week)
- Marlin, orange roughy, bigeye tuna
Alcohol:
- No amount of alcohol is considered safe during pregnancy
- Can cause fetal alcohol spectrum disorders
- Affects brain development throughout pregnancy
Foods to Limit or Consume with Caution
Caffeine
Safe limit: 200mg per day (about 1-2 cups of coffee)
Sources to monitor:
- Coffee (95mg per 8oz cup)
- Tea (25-50mg per 8oz cup)
- Chocolate (5-35mg per serving)
- Energy drinks (varies widely)
- Some medications and supplements
☕ Managing Caffeine Intake
- Switch to decaf coffee or herbal teas
- Mix regular and decaf coffee
- Choose smaller cup sizes
- Read labels on sodas and energy drinks
- Consider caffeine-free alternatives like chicory coffee
Deli Meats and Hot Dogs
Risk: Listeria contamination
Safe preparation: Heat until steaming hot (165°F internal temperature)
Alternatives: Freshly cooked meats, canned meats, vegetarian options
Certain Fish
Limit to 2-3 servings per week:
- Salmon, sardines, anchovies (low mercury, high omega-3s)
- Shrimp, crab, lobster (cooked thoroughly)
- Canned light tuna (limit to 12oz per week)
Unwashed Produce
Risk: Toxoplasmosis, E. coli, Salmonella
Safe practices:
- Wash all fruits and vegetables thoroughly
- Use a produce brush for firm produce
- Remove damaged or bruised areas
- Avoid pre-cut fruits and vegetables when possible
Questionable Foods: Case-by-Case Decisions
| Food Item | Risk Level | Safe Preparation | Recommendation |
|---|---|---|---|
| Soft-serve ice cream | Low-Medium | From reputable establishments | Generally safe, use judgment |
| Sprouts (alfalfa, bean) | Medium | Cook thoroughly | Avoid raw, cook if desired |
| Herbal teas | Varies | Research specific herbs | Stick to pregnancy-safe varieties |
| Honey | Low | Pasteurized honey | Safe for pregnant women |
| Artificial sweeteners | Low-Medium | FDA-approved varieties | Moderate use is generally safe |
Safe Food Handling Practices
Kitchen Safety Guidelines:
- Wash hands frequently: Before and after handling food
- Separate raw and cooked foods: Use different cutting boards
- Cook to proper temperatures: Use a food thermometer
- Refrigerate promptly: Don't leave perishables out more than 2 hours
- Clean surfaces: Sanitize counters and utensils regularly
Safe Internal Temperatures:
- Poultry: 165°F
- Ground meat: 160°F
- Beef, pork, lamb: 145°F with 3-minute rest
- Fish: 145°F or until flesh is opaque
- Eggs: Cook until yolk and white are firm
⚠️ Signs of Foodborne Illness
Contact your healthcare provider immediately if you experience:
- Severe nausea, vomiting, or diarrhea
- Fever above 101°F
- Severe abdominal cramping
- Signs of dehydration
- Flu-like symptoms after eating questionable food
Healthy Alternatives and Substitutions
Instead of Raw Fish:
- Cooked sushi rolls (California roll, cooked shrimp)
- Vegetarian sushi options
- Grilled or baked fish
- Canned salmon or sardines
Instead of Deli Meats:
- Freshly cooked and sliced turkey or chicken
- Canned chicken or tuna
- Hummus or avocado for sandwiches
- Heated deli meats (until steaming)
Instead of Soft Cheeses:
- Hard cheeses (cheddar, Swiss, parmesan)
- Pasteurized soft cheeses (check labels)
- Cottage cheese and ricotta (pasteurized)
- Cream cheese (usually pasteurized)
Instead of High-Caffeine Drinks:
- Herbal teas (pregnancy-safe varieties)
- Decaffeinated coffee
- Sparkling water with fruit
- Fresh fruit juices (pasteurized)
Dining Out Safely
Restaurant Guidelines:
- Ask questions: About preparation methods and ingredients
- Choose reputable establishments: With good food safety practices
- Avoid buffets: Food may sit at unsafe temperatures
- Order well-cooked items: Avoid rare or undercooked foods
- Skip the extras: Raw sprouts, unpasteurized dressings
Safe Restaurant Choices:
- Grilled or baked proteins
- Steamed vegetables
- Cooked pasta dishes
- Soups (if heated thoroughly)
- Fresh salads (ask about washing practices)
🎯 The Bottom Line on Food Safety
While the list of foods to avoid might seem overwhelming, remember that most foods are safe when properly prepared. Focus on eating a variety of well-cooked, properly handled foods. When in doubt, choose the safer option or consult your healthcare provider. The goal is reducing risk while still enjoying a nutritious, satisfying diet.
📱 Helpful Resources
For the most current food safety guidelines during pregnancy, consult:
- Your healthcare provider
- FDA pregnancy food safety guidelines
- CDC recommendations for pregnant women
- Academy of Nutrition and Dietetics resources

8. Managing Common Pregnancy Symptoms
Pregnancy brings many physical changes that can affect your appetite, digestion, and overall relationship with food. Understanding how to manage these symptoms through nutrition can significantly improve your comfort and ensure adequate nutrition throughout pregnancy.
Morning Sickness and Nausea
Despite its name, morning sickness can occur at any time of day and affects up to 80% of pregnant women, typically during the first trimester.
🤢 Nutritional Strategies for Morning Sickness
Foods That May Help:
- Ginger: Tea, candies, or supplements (consult your doctor first)
- Bland carbohydrates: Crackers, toast, rice, bananas
- Cold foods: Often better tolerated than hot foods
- Protein-rich snacks: May help stabilize blood sugar
- Sour foods: Lemon water, sour candies may provide relief
Eating Strategies:
- Eat before getting up: Keep crackers by your bedside
- Small, frequent meals: Every 2-3 hours to prevent empty stomach
- Stay hydrated: Sip fluids between meals, not during
- Avoid triggers: Strong smells, spicy, fatty, or very sweet foods
- Don't force foods: Eat what you can tolerate
When Morning Sickness is Severe (Hyperemesis Gravidarum):
- Inability to keep food or fluids down
- Weight loss of more than 5% of pre-pregnancy weight
- Signs of dehydration
- Requires medical intervention and possibly IV fluids
Heartburn and Acid Reflux
Heartburn affects up to 80% of pregnant women, especially in the second and third trimesters, due to hormonal changes and pressure from the growing uterus.
🔥 Managing Pregnancy Heartburn
Dietary Modifications:
- Avoid trigger foods: Spicy, acidic, fatty, or fried foods
- Eat smaller meals: 6-8 small meals instead of 3 large ones
- Chew thoroughly: Take time to eat slowly
- Stay upright: Don't lie down for 2-3 hours after eating
- Limit fluids with meals: Drink between meals instead
Foods That May Help:
- Oatmeal and other whole grains
- Non-citrus fruits (bananas, melons)
- Vegetables (except tomatoes and onions)
- Lean proteins
- Low-fat dairy products
- Ginger tea
Foods to Avoid:
- Citrus fruits and juices
- Tomato-based products
- Chocolate
- Caffeine
- Spicy foods
- Fried and fatty foods
Constipation
Constipation affects up to 40% of pregnant women due to hormonal changes, iron supplements, and pressure from the growing uterus.
💩 Relieving Pregnancy Constipation
Dietary Solutions:
- Increase fiber gradually: 25-35 grams per day
- Drink plenty of water: At least 8-10 glasses daily
- Add prunes: Natural laxative effect
- Include probiotics: Yogurt, kefir, fermented foods
- Choose whole grains: Brown rice, whole wheat bread, oats
High-Fiber Foods:
- Fruits: Apples with skin, pears, berries, prunes
- Vegetables: Broccoli, Brussels sprouts, artichokes, beans
- Grains: Oats, quinoa, brown rice, whole wheat products
- Legumes: Lentils, chickpeas, black beans
- Nuts and seeds: Chia seeds, flaxseeds, almonds
Lifestyle Modifications:
- Regular gentle exercise (walking, swimming)
- Establish regular bathroom routine
- Don't delay when you feel the urge
- Consider switching iron supplements if they worsen constipation
Food Aversions and Cravings
Up to 85% of pregnant women experience food aversions, while cravings affect 50-90% of pregnant women.
Managing Food Aversions:
- Don't force disliked foods: Find alternative nutrient sources
- Try different preparations: Raw vs. cooked, different seasonings
- Mask flavors: Add to smoothies or mixed dishes
- Wait it out: Aversions often resolve after first trimester
- Focus on what you can eat: Any nutrition is better than none
Handling Cravings Wisely:
- Honor healthy cravings: Your body may be signaling nutrient needs
- Find healthier alternatives: Frozen yogurt instead of ice cream
- Practice moderation: Small portions of desired foods
- Combine with nutrition: Add fruit to ice cream, nuts to chocolate
- Stay hydrated: Sometimes thirst masquerades as cravings
🚨 Unusual Cravings (Pica)
If you crave non-food items (ice, starch, dirt, etc.), contact your healthcare provider immediately. This condition, called pica, may indicate nutritional deficiencies and can be harmful.
Fatigue and Low Energy
Fatigue is common, especially in the first and third trimesters, due to hormonal changes and increased energy demands.
Nutritional Energy Boosters:
- Eat regular meals: Maintain stable blood sugar levels
- Include protein: At every meal and snack for sustained energy
- Choose complex carbs: Whole grains provide steady energy
- Stay hydrated: Dehydration worsens fatigue
- Iron-rich foods: Prevent anemia-related fatigue
- B-vitamin foods: Support energy metabolism
Energy-Sustaining Snack Ideas:
- Apple slices with almond butter
- Greek yogurt with berries and granola
- Whole grain crackers with cheese
- Trail mix with nuts and dried fruit
- Hummus with vegetable sticks
- Hard-boiled egg with whole grain toast
Swelling (Edema)
Mild swelling in feet, ankles, and hands is normal, especially in the third trimester, but excessive swelling may indicate complications.
Nutritional Management:
- Moderate sodium intake: Don't eliminate completely, but avoid excess
- Stay hydrated: Paradoxically, drinking more water can reduce swelling
- Potassium-rich foods: Bananas, potatoes, spinach help balance fluids
- Avoid processed foods: Often high in sodium
- Elevate feet: When resting
⚠️ When Swelling is Concerning
Contact your healthcare provider immediately if you experience:
- Sudden, severe swelling
- Swelling in face or around eyes
- Swelling accompanied by headache or vision changes
- Rapid weight gain (more than 2 pounds in a week)
These may be signs of preeclampsia, a serious pregnancy complication.
Gestational Diabetes
Gestational diabetes affects 2-10% of pregnancies and requires careful blood sugar management through diet and sometimes medication.
Dietary Management Principles:
- Consistent carbohydrate intake: Same amount at same times daily
- Choose complex carbohydrates: Whole grains, vegetables, legumes
- Pair carbs with protein: Helps stabilize blood sugar
- Eat regular meals: Don't skip meals or snacks
- Monitor blood sugar: As directed by healthcare provider
- Stay active: Gentle exercise helps control blood sugar
📊 Blood Sugar Management
If diagnosed with gestational diabetes, work with a registered dietitian and use our Calorie Calculator and Macro Calculator to help plan appropriate portions and timing of meals.
Creating Your Symptom Management Plan
Track Your Symptoms:
- Keep a food and symptom diary
- Identify trigger foods and helpful foods
- Note timing patterns
- Share findings with your healthcare provider
Build Your Toolkit:
- Stock up on foods that help your specific symptoms
- Prepare easy-to-digest meals in advance
- Have backup options for difficult days
- Create a support system for meal preparation
🌟 Remember: This Too Shall Pass
Most pregnancy symptoms are temporary and will resolve after delivery. Focus on managing symptoms while maintaining adequate nutrition. Don't hesitate to reach out to your healthcare provider if symptoms become severe or interfere with your ability to eat and stay hydrated.

9. Special Dietary Considerations
Every pregnancy is unique, and some women have special dietary needs due to medical conditions, food allergies, cultural preferences, or lifestyle choices. Understanding how to maintain optimal nutrition in these situations ensures both maternal and fetal health.
Vegetarian and Vegan Pregnancies
Well-planned vegetarian and vegan diets can be healthy during pregnancy, but require careful attention to certain nutrients that are more abundant in animal products.
🌱 Key Nutrients for Plant-Based Pregnancies
Vitamin B12:
- Critical need: Not found in plant foods
- Supplementation: Essential for vegans, recommended for vegetarians
- Sources: Fortified nutritional yeast, plant milks, supplements
- Daily need: 2.6 mcg during pregnancy
Iron:
- Plant sources: Lentils, chickpeas, spinach, quinoa, fortified cereals
- Absorption enhancers: Vitamin C foods (citrus, tomatoes, bell peppers)
- Absorption inhibitors: Tea, coffee, calcium (separate timing)
- Consider supplements: If blood levels are low
Omega-3 Fatty Acids:
- Plant sources: Flaxseeds, chia seeds, walnuts, hemp seeds
- Algae supplements: Direct source of DHA for vegans
- Daily goal: 200-300mg DHA
Protein:
- Complete proteins: Quinoa, buckwheat, hemp seeds, chia seeds
- Protein combining: Beans + grains, nuts + seeds
- Daily need: 71g during pregnancy
Sample Vegan Pregnancy Day:
- Breakfast: Fortified oatmeal with ground flaxseed, berries, and almond milk
- Snack: Hummus with vegetables and B12-fortified nutritional yeast
- Lunch: Quinoa bowl with chickpeas, tahini dressing, and leafy greens
- Snack: Smoothie with fortified plant milk, spinach, banana, and chia seeds
- Dinner: Lentil curry with brown rice and steamed broccoli
- Evening: Fortified plant milk with calcium and vitamin D
Food Allergies and Intolerances
Managing food allergies during pregnancy requires careful planning to ensure adequate nutrition while avoiding trigger foods.
Common Pregnancy-Safe Alternatives:
| Allergen | Nutritional Concern | Safe Alternatives | Key Nutrients |
|---|---|---|---|
| Dairy | Calcium, Vitamin D, Protein | Fortified plant milks, leafy greens, sardines | Calcium, Vitamin D, Protein |
| Eggs | Protein, Choline, Vitamin D | Meat, fish, legumes, choline supplements | Complete proteins, Choline |
| Fish/Shellfish | Omega-3s, Protein, Iodine | Algae supplements, walnuts, iodized salt | DHA, EPA, Iodine |
| Nuts | Healthy fats, Protein, Vitamin E | Seeds, avocado, olive oil | Healthy fats, Protein |
| Gluten | B vitamins, Fiber, Iron | Quinoa, rice, certified gluten-free products | B vitamins, Fiber |
🔍 Reading Labels During Pregnancy
- Check for hidden allergens in processed foods
- Look for "may contain" warnings
- Verify that alternatives are fortified with key nutrients
- Choose certified allergen-free products when available
- Work with a registered dietitian for meal planning
Gestational Diabetes Management
Gestational diabetes requires careful carbohydrate management to maintain healthy blood sugar levels while ensuring adequate nutrition for fetal growth.
Carbohydrate Management Strategies:
- Consistent timing: Eat meals and snacks at the same times daily
- Portion control: Measure carbohydrate portions carefully
- Choose complex carbs: Whole grains, vegetables, legumes
- Pair with protein: Helps slow glucose absorption
- Monitor blood sugar: Test as directed by healthcare provider
Sample Gestational Diabetes Meal Plan:
- Breakfast: 1 slice whole grain toast + 2 eggs + 1/2 avocado
- Mid-morning: 1 small apple + 1 oz cheese
- Lunch: 2 oz grilled chicken + 1/2 cup brown rice + mixed vegetables
- Afternoon: 1/4 cup nuts + 1 small orange
- Dinner: 3 oz salmon + 1 small sweet potato + green salad
- Evening: 1 cup milk + 2 small cookies (if blood sugar allows)
⚠️ Gestational Diabetes Monitoring
Work closely with your healthcare team to:
- Monitor blood glucose levels as prescribed
- Track food intake and blood sugar responses
- Adjust meal plans based on glucose readings
- Consider medication if diet alone isn't sufficient
- Monitor baby's growth and development
Multiple Pregnancies (Twins, Triplets)
Carrying multiples significantly increases nutritional needs and requires careful monitoring of weight gain and nutrient intake.
Increased Nutritional Needs:
- Calories: Additional 600 calories/day for twins by second trimester
- Protein: 50g additional protein daily
- Folate: 1000 mcg daily (higher than singleton pregnancy)
- Iron: Often requires prescription supplements
- Calcium: 1500mg daily
Weight Gain Guidelines for Twins:
- Normal BMI: 37-54 pounds total
- Overweight BMI: 31-50 pounds total
- Obese BMI: 25-42 pounds total
- Pattern: More weight gain in first half of pregnancy
Teen Pregnancy Nutrition
Pregnant teenagers have unique nutritional needs as they're still growing themselves while supporting fetal development.
Special Considerations:
- Higher caloric needs: Growing adolescent + pregnancy demands
- Calcium emphasis: Peak bone-building years
- Iron focus: Higher risk of anemia
- Weight gain: Often at upper end of recommendations
- Social support: Family involvement in meal planning
Pregnancy After Bariatric Surgery
Women who have had weight loss surgery require specialized nutritional monitoring during pregnancy.
Key Monitoring Areas:
- Vitamin B12: Absorption may be impaired
- Iron: Higher risk of deficiency
- Folate: Ensure adequate intake
- Protein: May need higher amounts
- Weight gain: May require modified guidelines
Cultural and Religious Dietary Practices
Many cultural and religious dietary practices can be safely maintained during pregnancy with some modifications.
Common Considerations:
- Fasting practices: May need modification during pregnancy
- Food restrictions: Ensure adequate nutrition from allowed foods
- Traditional foods: Incorporate nutrient-dense cultural foods
- Preparation methods: Ensure food safety practices
- Community support: Involve family in healthy meal planning
🤝 Working with Healthcare Providers
For any special dietary situation during pregnancy:
- Inform your healthcare provider about dietary restrictions
- Consider working with a registered dietitian
- Monitor nutrient levels through blood tests
- Adjust supplement regimens as needed
- Don't hesitate to ask questions about safety
🎯 The Key to Success
Regardless of your special dietary needs, the key to a healthy pregnancy is planning, monitoring, and working with qualified healthcare professionals. Most dietary restrictions can be successfully managed during pregnancy with proper attention to nutrition and regular monitoring.
10. Preparing for Postpartum Nutrition
The fourth trimester - the first three months after birth - brings new nutritional challenges and opportunities. Whether you're breastfeeding or not, your body needs proper nutrition to recover from pregnancy and childbirth while adapting to the demands of caring for a newborn.
Immediate Postpartum Recovery (First 6 Weeks)
Your body undergoes significant changes as it recovers from pregnancy and childbirth. Proper nutrition supports healing, energy levels, and emotional well-being during this critical period.
Nutritional Priorities for Recovery:
- Protein: Support tissue repair and wound healing
- Iron: Replenish stores after blood loss during delivery
- Vitamin C: Enhance wound healing and iron absorption
- Zinc: Support immune function and tissue repair
- Hydration: Essential for healing and milk production
- Fiber: Prevent constipation, especially after C-section
🍲 Easy Recovery Meals
Prepare these nutrient-dense, easy-to-eat meals during your third trimester:
- Freezer soups: Lentil, chicken, or vegetable-based
- Overnight oats: Pre-made with protein powder and fruit
- Energy balls: Dates, nuts, seeds for quick energy
- Smoothie packs: Pre-portioned frozen fruits and vegetables
- One-pot meals: Casseroles, stews, grain bowls
Breastfeeding Nutrition
Breastfeeding requires additional calories and nutrients to support milk production while maintaining maternal health. Your nutritional needs are actually higher during breastfeeding than during pregnancy.
Increased Nutritional Needs While Breastfeeding:
| Nutrient | Pre-Pregnancy | Pregnancy | Breastfeeding | Increase from Pre-Pregnancy |
|---|---|---|---|---|
| Calories | 2000 | 2340-2450 | 2500-2700 | +500-700 |
| Protein (g) | 46 | 71 | 71 | +25 |
| Calcium (mg) | 1000 | 1000 | 1000 | Same |
| Iron (mg) | 18 | 27 | 9 | -9 (due to no menstruation) |
| Vitamin A (mcg) | 700 | 770 | 1300 | +600 |
| Vitamin C (mg) | 75 | 85 | 120 | +45 |
Hydration for Breastfeeding:
- Daily goal: 13 cups (104 oz) of fluids
- Listen to thirst: Your body will signal increased needs
- Keep water nearby: During nursing sessions
- Variety counts: Water, milk, herbal teas, soups
- Monitor urine: Should be pale yellow
🥛 Foods That Support Milk Production
While no food can guarantee increased milk supply, these nutrient-dense options support overall lactation:
- Oats: Rich in iron and fiber
- Salmon: Omega-3s for brain development
- Eggs: Complete protein and choline
- Leafy greens: Folate, iron, calcium
- Nuts and seeds: Healthy fats and protein
- Avocados: Healthy fats and fiber
- Sweet potatoes: Beta-carotene and complex carbs
Foods to Limit While Breastfeeding:
- Alcohol: Passes into breast milk; time consumption carefully
- Caffeine: Limit to 1-2 cups coffee daily; baby may be sensitive
- High-mercury fish: Continue pregnancy restrictions
- Highly processed foods: Provide fewer nutrients for milk production
Formula Feeding Nutrition
If you're formula feeding, your nutritional needs return closer to pre-pregnancy levels, but recovery nutrition remains important.
Post-Pregnancy Recovery Focus:
- Gradual calorie reduction: Return to pre-pregnancy needs over time
- Continue prenatal vitamins: For 6-8 weeks postpartum
- Iron-rich foods: Replenish stores after delivery
- Balanced meals: Support energy and mood stability
- Adequate sleep support: Magnesium, B vitamins
Postpartum Weight Loss
Healthy postpartum weight loss focuses on gradual changes that support energy levels and overall well-being.
Safe Weight Loss Guidelines:
- Timeline: Wait 6-8 weeks before focusing on weight loss
- Rate: 1-2 pounds per week maximum
- Breastfeeding: No less than 1800 calories daily
- Formula feeding: No less than 1500 calories daily
- Focus on nutrition: Quality over restriction
⚠️ Avoid These Postpartum Diet Mistakes
- Extreme calorie restriction: Can affect milk supply and energy
- Eliminating food groups: May lead to nutrient deficiencies
- Diet pills or supplements: Not safe while breastfeeding
- Skipping meals: Can cause blood sugar crashes and overeating
- Comparing to others: Every body recovers differently
Managing Postpartum Challenges
Sleep Deprivation and Nutrition:
- Prepare easy meals: Batch cook during pregnancy
- Keep healthy snacks accessible: Nuts, fruit, yogurt
- Accept help: Let others cook or bring meals
- Stay hydrated: Dehydration worsens fatigue
- Avoid sugar crashes: Choose complex carbs over simple sugars
Postpartum Mood and Nutrition:
- Omega-3 fatty acids: Support brain health and mood
- B vitamins: Important for energy and neurotransmitter production
- Vitamin D: Deficiency linked to postpartum depression
- Regular meals: Stable blood sugar supports mood stability
- Limit alcohol: Can worsen mood and interfere with sleep
Meal Planning for New Parents
Third Trimester Meal Prep for Postpartum:
- Double recipes: Freeze half for later
- One-handed foods: Smoothies, energy bars, wraps
- Slow cooker meals: Set and forget options
- Freezer breakfast burritos: Quick, nutritious starts to the day
- Lactation cookies: If planning to breastfeed
Postpartum Meal Ideas:
| Meal | Quick Option | Make-Ahead Option | Key Nutrients |
|---|---|---|---|
| Breakfast | Greek yogurt parfait | Overnight oats | Protein, probiotics, fiber |
| Lunch | Avocado toast with egg | Freezer soup | Healthy fats, protein, fiber |
| Dinner | Rotisserie chicken salad | Freezer casserole | Protein, vegetables, complex carbs |
| Snacks | Apple with nut butter | Energy balls | Fiber, healthy fats, protein |

Supplements During Postpartum
Continue Taking:
- Prenatal vitamins: For 6-8 weeks minimum, longer if breastfeeding
- Vitamin D: Especially important if breastfeeding
- Omega-3s: Support mood and brain health
- Iron: If levels are low after delivery
Consider Adding:
- Probiotics: Support digestive and immune health
- Vitamin B12: If vegetarian/vegan or showing deficiency
- Magnesium: Support sleep and muscle recovery
🤱 Remember: You're Still Recovering
Your body has done incredible work growing and delivering a baby. Give yourself time to heal and adjust. Focus on nourishing foods, adequate hydration, and rest when possible. Don't hesitate to ask for help with meal preparation and household tasks.
📞 When to Seek Help
Contact your healthcare provider if you experience:
- Persistent fatigue that doesn't improve with rest
- Signs of postpartum depression or anxiety
- Difficulty maintaining adequate nutrition
- Concerns about milk supply (if breastfeeding)
- Unusual food cravings or aversions
📋 Key Takeaways
- Start early: Begin taking prenatal vitamins before conception if possible
- Focus on quality: Choose nutrient-dense foods over empty calories
- Stay consistent: Regular meals and snacks support stable blood sugar
- Listen to your body: Appetite and food preferences will change
- Stay hydrated: Adequate fluid intake is crucial throughout pregnancy
- Plan ahead: Meal planning makes healthy eating easier
- Seek support: Work with healthcare providers and registered dietitians
- Be flexible: Adapt your nutrition plan as your pregnancy progresses
🌟 Final Thoughts
Pregnancy nutrition doesn't have to be perfect to be effective. Focus on making the best choices you can with the information and resources available to you. Every healthy meal and snack is a gift to your growing baby and yourself. Trust your body, work with your healthcare team, and remember that you're doing an amazing job growing a new life.
For personalized nutrition advice, always consult with your healthcare provider or a registered dietitian who specializes in prenatal nutrition. They can help you create a plan that meets your individual needs and circumstances.
Congratulations on your pregnancy journey, and here's to a healthy, well-nourished nine months ahead!